Mpox: A Growing Emergency on the African Continent
It is imperative that the international community raise awareness and proactively address and prevent the spread of infectious diseases. In August 2024, the Africa Centers for Disease Control and Prevention (CDC) and World Health Organization declared the surge of the new strain of mpox in the Democratic Republic of the Congo (DRC) and other African countries as a public health emergency of continental security and international concern respectively. Within 12 African countries, there have been 18,737 (3,101 confirmed and 15,636 suspected) cases and 541 deaths resulting from the mpox virus in 2024 (Africa Centers for Disease Control and Prevention, Epidemic Intelligence Report, August 16, 2024).
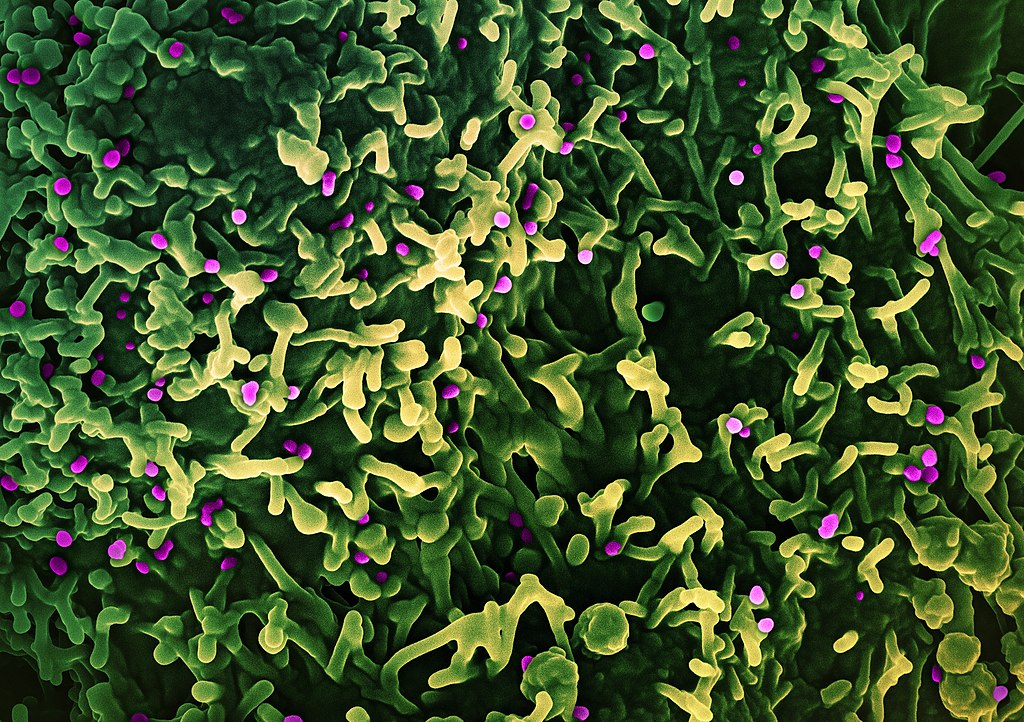
While the majority of reported cases are in the DRC, where the new Clade I strain is responsible for the outbreak, it’s crucial to be vigilant to prevent the further spread of disease within the continent. According to the Africa CDC, 16,794 (2,860 confirmed and 14,934 suspected) cases and 535 deaths in DRC this year. Children under the age of 15 account for 82% of the deaths, making them the most affected group. Additionally, the Republic of the Congo and Kenya are now among several African nations with confirmed cases of the new strain, which is more transmissible and lethal and the first known strain to be sexually transmissible. It can be transmitted through physical contact with an infected person, object, animal, bodily fluids, and respiratory secretions.
The Community of Disciples of Christ in Congo (CDCC) in the DRC and healthcare systems in other African countries have encountered significant challenges and barriers in mitigating the spread of MPOX, including:
- There has been limited or minimal access or availability of vaccines.
- Expanding outreach and disease awareness campaigns are still needed, primarily in remote areas where people continue to handle bush meat.
- Existing health structures have not been strengthened, and there has been a shortage of protective equipment within most hospitals.
In 2022, there was an international mpox outbreak in non-endemic countries caused by the Clade II strain. Developed nations achieved disease control by mid-2023 through effective awareness campaigns, diagnostic testing, and vaccines. And in May 2023, the World Health Organization announced that the international mpox emergency had ended. However, mpox infections, caused by the emergence of a more virulent Clade I strain, continued to rise in DRC, driven by the lack of equitable resources. And currently, the nation is addressing a significant increase in mpox infections and transmission to neighboring and nearby countries, including Kenya, which had not previously reported any cases of the disease.
Although public health officials report that the number of mpox cases is rising, the CDCC reports that the number of mpox cases in their healthcare facilities has declined over the past month, which include Lotumbe Hospital, Bolenge Hospital, Modombe Hospital, Wema Hospital, and Monieka Hospital. Unfortunately, two of their physicians, one at Bolenge Hospital and the other at Lotumbe Hospital, were infected with mpox and are recovering. Despite this challenge, the CDCC plans to implement programs to raise awareness in remote areas, capacitate their health care facilities, and strengthen their ability to respond to mpox emergencies.
Republic of the Congo (RC)
At the submission of this report, there has been a reported total of 150 suspected mpox infections, 19 confirmed infections, and one death in the Republic of Congo (Africa Centers for Disease Control and Prevention, August 16, 2024). And more than 80% of those cases have been reported from the northern region of the country, according to the RC Ministry of Health and Population.
The Disciples of Christ Church of the Congo, Brazzaville’s main concern is the potential for greater spread of the infection, particularly to the ecclesial posts of Loukoléla, Liranga, and Impfondo. These posts are more vulnerable because they are in remote areas that are less developed, and citizens interact and commute within the most affected areas. Thus, their first response is to engage in multi-sector collaborative efforts to contain the spread of disease by implementing awareness campaigns to educate local communities about mpox, and prevention strategies, and to dispel myths. Subsequent actions will be determined by disease transmission.
Angola and Zambia
I have communicated with partners in Angola and Zambia, and they have reported no impacts of mpox and that this is not a prevalent concern within their communities at this time. Still, they are taking precautions and will update us on any developments.
South Sudan
Communications with our partner in South Sudan, the South Sudan Council of Churches, have been challenging. As of now, we have yet to receive a response to our inquiries.
Kenya
Kenya reported its first mpox case at the end of July 2024. However, I have communicated with our partners, and they report no impact within the communities they serve.
In conclusion, the mpox public health emergency continually develops and requires urgent attention. Therefore, it is paramount that we work to achieve equitable access to mpox testing, vaccines, medications, and protective equipment on the continent to fight mpox across affected countries and mitigate the further spread of infection on the continent.
Global Ministries continues to support and accompany our partners in their efforts to respond to the public health emergency.
by Dr. Kahala Cannon, Global Relations Minister, Africa